Eggs are more prone to genetic abnormalities as a woman ages. These abnormalities lead to increased incidences of infertility, miscarriage and birth defects especially in women over 38 years of age. Egg freezing is a method that suspends egg aging. Since the genetic status of an egg cannot be determined solely on appearance, methods to evaluate eggs using genetic probes have developed and recently tested.
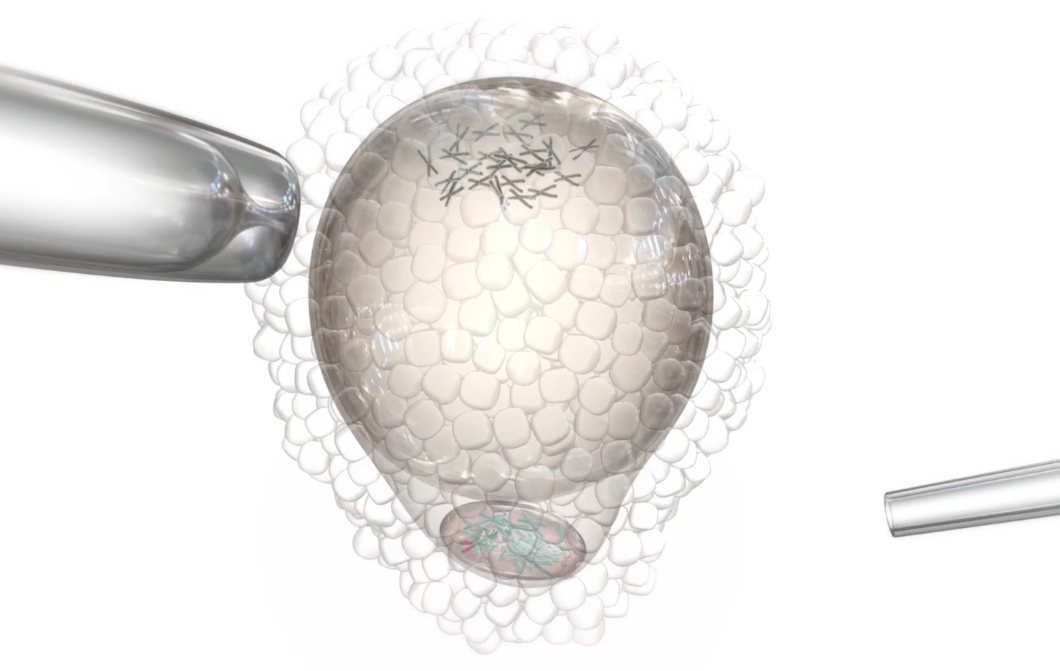
The egg discards DNA at two different times during its development, ovulation and fertilization. The reason for this is to reduce the number of chromosomes to 23 in order to match the 23 chromosomes delivered by the sperm. The discarded DNA (in the form of excess chromosomes) is jettisoned outside of the egg as a small, round pocket called the polar body. Removal of the polar body (biopsy) can provide useful information about the genetic status of the egg. For example, if 23 chromosomes are found in the polar body, the presumption is that a normal count of 23 chromosomes remains in the egg. In contrast, if a number other than 23 is found in the polar body, it implies that an abnormal count remains in the egg and suggests that the egg and ensuing embryo will be genetically abnormal. Testing of the polar body using modern genetic techniques such as Comparative Genomic Hybridization (CGH) or Array-CGH, allows identification of abnormal eggs and can thus help determine the number of genetically normal eggs a woman has to freeze.
However, there are several important limitations to this technology. First, CGH and Array-CGH are still considered experimental, with very little clinical data available. Most clinical data is based on young egg donors and does not reflect the genetic status of eggs from women in their late 30’s. Second, embryos may be genetically abnormal due to mistakes contributed by the egg at the time of the first polar body formation or the second polar body formation; or mistakes contributed by the sperm at the time of fertilization. Therefore, assessing only the first polar body by no means guarantees that a normal embryo will derive. Third, and perhaps most concerning, is the lack of research regarding the effects of biopsying an egg prior to freezing.
We recently completed a small clinical trial wherein we performed polar body biopsy on eggs prior to freezing. We found a high degree of egg damage. The panel of microscopic pictures above demonstrate these changes: the first picture is a normal egg with an intact first polar body (Photo #1); the next picture is an egg after the polar body was removed (Photo #2); the next two pictures show a biopsied egg after freezing and thawing demonstrating egg contents (Photos #3 & #4) extruding through the biopsy slit. 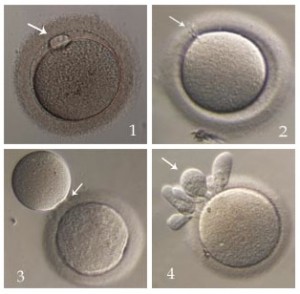 These changes were found on multiple eggs from different patients. These eggs had to be discarded. In addition, many other eggs demonstrated abnormal chromosome segregation after fertilization, and none of the patients achieved a pregnancy.
These changes were found on multiple eggs from different patients. These eggs had to be discarded. In addition, many other eggs demonstrated abnormal chromosome segregation after fertilization, and none of the patients achieved a pregnancy.
At the current time we do not recommend polar body biopsy of eggs prior to freezing until further studies on effectiveness and safety are available.