Two Merck drugs for treating male baldness and enlarged prostate will now carry extended labels to add more possible sexual side effects, US regulators said.
Tag: fertility
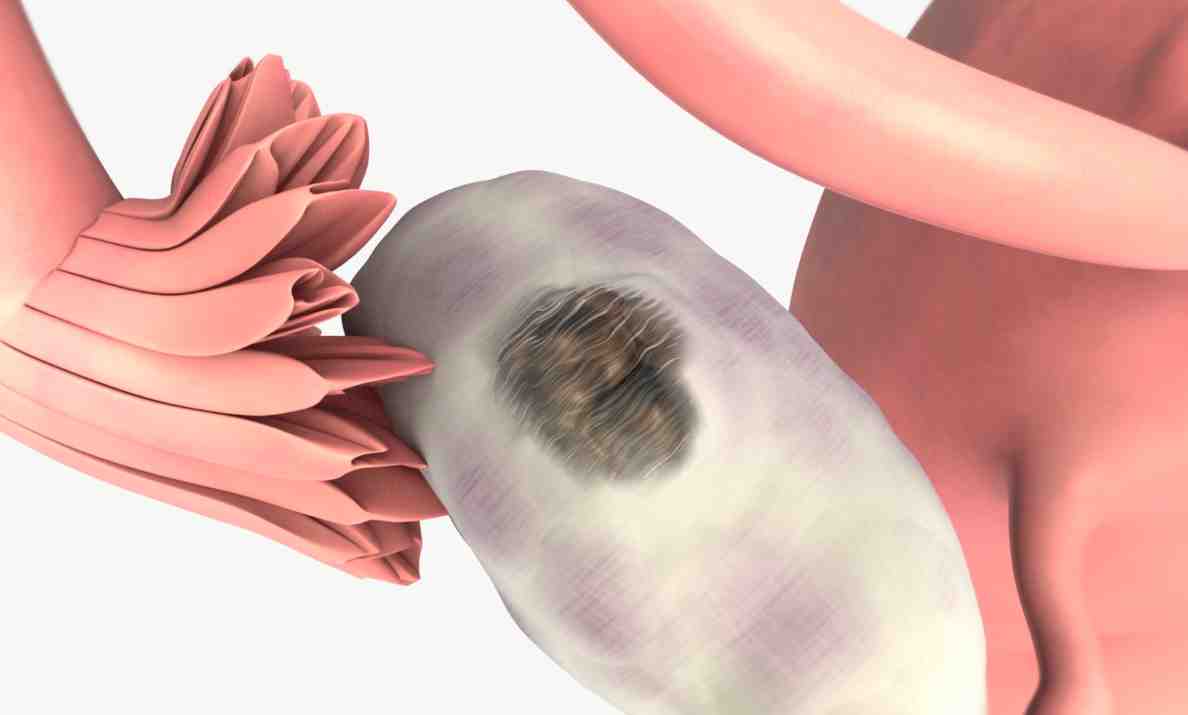
What Is Polycystic Ovary Syndrome
- Irregular or skipped menstrual periods
- Obesity and difficulty controlling weight gain
- Male pattern hair growth
- Acne and other chronic skin conditions
- Dark brown or black patches on the skin
Polycystic Ovary Syndrome and Infertility
PCOS is the most common hormonal abnormality causing infertility in women. It affects fertility by suppressing ovulation. Egg follicles may begin to mature but do not ovulate or release the egg into the fallopian tube. These follicles remain as cysts in the ovaries. In women with PCOS, the ovaries also produce excessive amounts of testosterone (male hormone) that can lead to acne and hair growth. In the fat cells, testosterone is converted to estrogen, leading to excessive buildup of the uterine lining which may contribute to heavy or irregular bleeding.Fertility Treatment for PCOS
High levels of insulin associated with obesity interfere with ovulation and also worsen PCOS symptoms. Minimizing insulin resistance via a healthy, safe weight loss regimen is a common first step for patients with PCOS who want to make conception more likely. Insulin regulating medications may also be prescribed. Some women are able to begin ovulating more normally at this point and may be able to conceive naturally.Fertility enhancing drugs such as Clomid, Metformin and gonadotropins may be used to stimulate ovulation. This approach is tried after other potential causes of infertility have been ruled out. In-Vitro-Fertilization can also be used for some women with PCOS. by: Dr. John Jain
Gel to Boost Male Fertility Being Developed
Male fertility has been largely overlooked until recently with most treatments requiring women to take medication or undergo expensive and invasive procedures.
Why aren’t more young cancer patients preserving their fertility?
The answer to the question above, according to a recent study in the journal Cancer, is that too often, young women who have cancer simply don’t understand their options when it comes to preventing the loss of their chance to have a child or more children. According to Reuters Health, which reported on the new research late last month, only one in every 25 women who was diagnosed with one of five types of cancer since the early 1990s opted to freeze eggs or embryos prior to cancer treatment — in spite of the fact that 47 to 63 percent said they wanted to have a child or children.
This finding is the result of research on 1,000 women in California ages 18 to 40 who’d been diagnosed with cancer between 1993 and 2007. Sixty-one percent of the women said their doctors talked to them about how cancer treatment could affect their chances of having a baby and how they could preserve their fertility — which means that 39 percent of patients didn’t get that guidance. Just four percent of those who got counseling about fertility preservation took action – by freezing eggs or embryos before, say, they underwent chemotherapy or radiation.
The research found, not surprisingly, that the women who had been counseled about how to save their fertility, or minimize the impact of treatment on their ability to conceive, were much less likely to feel regret later, versus the women who’d never talked to a doctor about their options for having a child or children later before undergoing treatment. Though the most recent data is still five years old, there’s reason to believe we still have a bit to go before all young women who get a cancer diagnosis are aware of all their options for having a family as they consider the treatment plan that’s right for them.
Provinces Better Off Without Federal Oversight of Fertility Treatments
On the heels of news that the federal government plans to eliminate the only agency that governs fertility treatments, a new study from the University of Calgary suggests the provinces might be better off without the federal oversight.
Scientists to Apply for License to Fertilize Human Eggs Grown in Laboratory
Scottish scientists are set to revolutionise fertility treatment following the development of a new technique that could lead to a reversal of the menopause in older women.
Looking for the right surrogate? A new site rates surrogacy agencies
We recently read about the launch of Surrogacy Advisor, a new site that offers ratings of surrogacy agencies from parents who’ve used a surrogate to carry their child. The site also includes reviews and ratings of fertility clinics.
Surrogacy Advisor appears to be just getting started, so there’s definitely not a comprehensive list of agencies and clinics represented (and some are outside the U.S.), but over time it could become a valuable tool to help would-be parents who are looking for a reputable surrogate or a clinic to work with — one that others in their situation rated highly. At press time, just 11 surrogacy agencies had ratings, with between three and 22 reviews for each. You can see the average cost for surrogacy at each rated agency, and how long the surrogacy “journey” took, on average, in months.
For fertility clinics, you can see a clinic’s overall score (based on a survey completed by parents who used it), the total number of reviews (at press time, CT Fertility had the highest rating, and also the greatest number of reviews – 26, compared to as few as three for many clinics — though only 10 clinics were listed, including a few outside the U.S.), as well as the percentage of patients who filled out the survey who conceived on the first cycle.
If you’re a prospective parent you can click here to complete a survey for an agency, and the site includes videos and articles about surrogacy as well.
Would you use a service like Surrogacy Advisor?
African American women are more likely to experience infertility
The release goes on to note that black women are less likely to seek the help of a fertility specialist or assisted reproductive techniques (ART) like in vitro fertilization (IVF) or intrauterine insemination (IUI). Possible reasons, says Dr. McCarthy-Keith, are that the cost of treating infertility may be prohibitively high — for black couples as well as those from any ethnic background — and that limited awareness of treatment options and/or access to fertility specialists may hinder black women getting help that would allow them to conceive, carry, and deliver a healthy baby.
Black women may be more medically challenged, too, owing to much higher rates of uterine fibroids, which can impair a woman’s odds of conceiving.
Prevention: HPV Vaccine Shows Reduced Recurrence
A new study suggests that the vaccine against human papillomavirus can significantly cut the likelihood of virus-related disease even among women who have had surgery for cervical cancer caused by HPV.
Can Bicycling Affect a Woman’s Sexual Health?
Spending time on a bicycle seat, which has been linked to erectile dysfunction in men, may also be a hazard to a woman’s sexual health, a new study shows.